Case study: treating a UTI with Chlorine Dioxide
A friend shares her experience of effectively treating a UTI without antibiotics
Urinary tract infections (UTIs) can be the bane of a woman’s existence. When she is younger and sexually active, they can be the result of frequent and enthusiastic sexual intercourse. When she is older and working in a demanding job, insufficiently hydrated, holding her urine for hours because she can’t get to the bathroom during the shift, UTIs can become a literal occupational hazard. When women are older and experiencing some degree of incontinence, using pads which absorb the urine, but maintain a warm and moist environment, encourages bacterial growth can contribute to UTIs. Patients regularly arrive in the Emergency Department (ED) from nursing homes with new onset confusion, recent falls, or a general downward trend in their health and a UTI is one of the most common reasons.
There is a basic physiological reason why women suffer UTIs more than men, and that is because the distance from the point of entry, the urethra, to the bladder via the urethra, is much shorter in a woman than in a man. Best medical practice would be to obtain a urine analysis with a reflex culture before prescribing antibiotics to any woman with UTI symptoms. Ubiquitous use of the ED and Urgent Care facilities can preclude this step. Many PCPs will only do a dipstick urine test in the office.
There are many reasons besides a UTI which would cause a woman to have lower abdominal discomfort, burning with urination, urinary frequency and urgency. If you have ever tried to argue with an 80-year-old about the need to do a urinalysis instead of just prescribing antibiotics, you intimately know the meaning of an uphill battle. Multiply that by hundreds and it can wear you down. The vast majority of the patients who we see in our practice at the Leading Edge Clinic, treating post acute sequelae of Covid and vaccine injury from the Covid shots, have some degree of mast cell activation. One common symptom of mast cell activation is interstitial cystitis That is inflammation and irritation of the lining of the bladder, which can lead to symptoms similar to a urinary tract infection. In fact, I have learned to ask patients during their initial visit if they have a history of interstitial cystitis as an important indicator of pre-existing mast cell activation.
A dear female friend who I shall call Daisy, recently developed symptoms of a urinary tract infection. She woke with urinary urgency, burning at her urethra upon urination, and an incomplete sense of emptying after voiding. She and her sexual partner literally cleaned up their act, and in spite being injured from two bad batch shots of Moderna, she was able to successfully avoid a UTI for the last 2 1/2 years. Unfortunately, this UTI followed directly on the heels of an enthusiastic session of lovemaking.
Because her PCP was not available due to a snow day, and the antibiotics he had previously prescribed her for such an occasion were expired, I agreed to order antibiotics and a medication which numbs the bladder in order to decrease discomfort, phenazopyridine. This is also available over the counter as AZO Urinary Pain Relief, Urispas or Urinary Pain Relief. She did not want to go out into a snow storm to the hospital to get lab testing of her urine, but I made a strong argument for it, and ultimately she went. Antibiotic resistance is real, and one of the values of getting a urinalysis with reflex culture is to determine if the bacteria causing the infection can be effectively treated with the chosen antibiotic, or if there is resistance, in which case a provider should guide the patient to switch to a more effective antibiotic.
Daisy picked up her prescription from the pharmacy after providing a urine sample to the local hospital lab. Then she had more questions and a decision to make. She had recently been reading about chlorine dioxide (CD) and was reluctant to start antibiotics. The reason for this is that she has had multiple issues with her teeth and gums since her vaccine injury from the Moderna shots, which required multiple rounds of strong antibiotics. Since those treatments she has been diligently trying to restore the the balance of her microbiome, using tools such as the pre-biotic fruit powder Baobab, and drinking raw milk. Her digestion had been off following the previous rounds of antibiotics and she used the peptide BPC 157, which isn’t cheap at $150 a month for three months.
Knowing that she had the option of starting the antibiotics at any time, Daisy decided to press forward with what is called Protocol 1000. A patient will mix one drop of sodium chlorite 22.5% with one drop of hydrochloric acid 4%, give it a minute to ripen, during which time it turns yellow, and starts to smell like bleach, which it isn’t. This newly formed yellow colored, gas-emitting drop is called one activated drop. She would then add 8 ounces of water and drink it right down. She endeavored to do this every hour for eight hours a day for the ensuing three weeks.
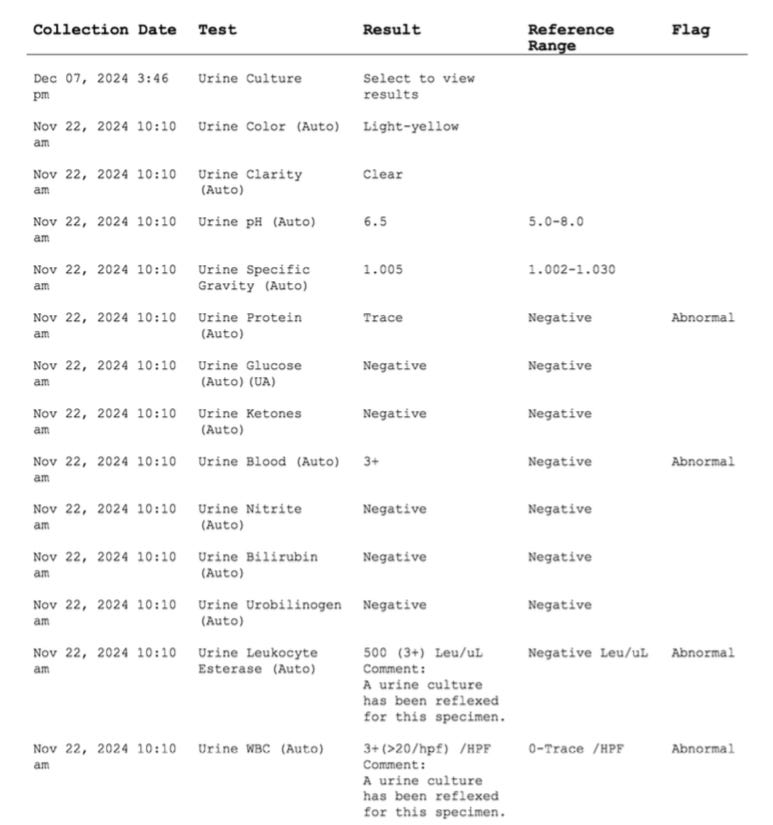
The urinalysis results came back in less than twenty four hours, and Daisy had confirmation of a UTI. She had 3+ blood, WBCs, and leukocyte esterase (and enzyme released from WBCs after they engulf, digest and excrete the remains of pathogens). She also had 1+ bacteria, and a reflex urine culture was initiated by the lab.
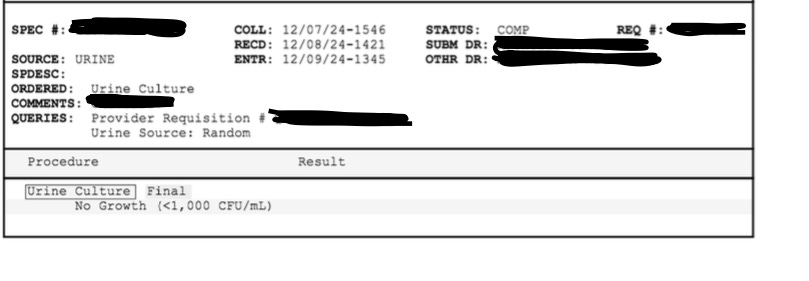
The culture came back positive for E. coli, which is the case in ~70-90% of UTIs in women due to the proximity of the anus to the vagina and urethra. E. coli also has specialized structures called fimbriae which enable it to adhere to the cells lining the urinary tract, which can make it difficult to flush out during urination. The nitrofurantoin (Macrobid) which I had prescribed would have effectively treated the bacteria, if she had chosen to use it.
I listened to her daily reports with keen interest, as I have never known a person who did this firsthand. It was neither easy nor a bed of roses. Within the first day or two, she developed diarrhea and her stools remained loose for about a week before firming up again. She had some abdominal discomfort, in particular during the first week, waking up with cramping, and this was on top of her slowly resolving UTI symptoms. Reviewing Protocol 1000, she clarified that she could increase the number of drops she took every hour from one to three. In week two, she tried going up to two drops and had some nausea. She then tried going up to three and had abdominal discomfort so went back to two for a couple days eventually landing on three drops per hour during the third week. In addition to physical symptoms, Daisy was anxious, because I couldn’t guide her based on my clinical experience with CD (having none at that point) and she has previously experienced a UTI, which deteriorated into an acute renal infection. At several points I reminded her that she had the antibiotic which I had ordered, and the culture had shown that it would treat the bacteria causing her UTI. Having this backup plan, she decided to continue in her personal experiment with CD. I will also add that because her appetite was off for at least the first week she found it challenging to know when she should take her supplements and medications or eat in relation to dosing with CD.
After the first week, the urinary tract infections had subsided significantly. Her appetite was slowly returning, her stools had firmed up, and she made an interesting observation. “I feel much more relaxed. I feel calmer. I’m not waking up with the usual morning headaches. I feel like whatever it’s doing, somehow the chlorine dioxide is healing me in other ways. “
I commented that before starting the CD, she knew she had 1.5 out of four amyloid fibrin micro clotting. This had been a dramatic reduction from her previous measurement of 3.5 out of 4 thanks to her consistent use of IVM, sulodexide, rapamycin, and Neprinol, which is a proprietary blend of nattokinase, serrapeptase, lumbrokinase, quercetin, and bromelain. Dr. Andreas Ludwige Kalcker, the German-born biophysical researcher who has written a great deal about chlorine dioxide solution (CDS), the more complicated cousin of CD, has an academic article which demonstrates micro clotting being treated with CDS, and 12 minutes later showing pristine and unencumbered red blood cells and platelets. This would point towards CD or CDS efficiently removing the fibrin amyloid tangles, which entrap the platelets and red blood cells. And, unlike prescription anticoagulants that we use, it would appear to spare the red blood cells and platelets enmashed in the micro clot.
I should also share that the patient had been making use of additional alternative therapies. The first was a Pure Encapsulations product which combines cranberry with D-Mannose. She opted to stop this after the first day, because it is profoundly antioxidant and could neutralize the CD. The second was a homeopathic remedy for UTI symptoms called Staphysagria; she used the 30C strength from Boiron, three pellets under the tongue three times daily. She weaned herself off the phenazopyridine and stopped using the homeopathic remedy towards the end of the third week. By the end of week two she was completely asymptomatic and feeling pretty confident in her cure. That was a Friday. Literally the next day she had a return of symptoms, awakening with burning upon urination and a sense of bladder discomfort. She was deeply deeply discouraged.
When she asked me for my advice, I said that I would be willing to write for another urinalysis so that she could confirm the symptoms were from a UTI. Unfortunately, when she went to the hospital, the lab was closed for the weekend and her next stop was the Urgent Care. By Urgent Care standards, her visit was speedy, courteous, and accomplished the goal of having a practitioner evaluate her. The treating Nurse Practitioner (NP) chided her for not starting her antibiotics when the UTI was first identified. She was also a little displeased that my Daisy had not told her about taking phenazopyridine, which turns the urine orange— and prevented them from doing a urine dipstick on site. Nevertheless, the NP could see the urine culture results from two weeks prior in the EMR system, which grew out E Coli, and prescribed a different antibiotic than what I had ordered.
The NP told Daisy that they would send the urine out for testing and that she should start the antibiotic right away, which she did. That was a Saturday. Sunday there were no results to be seen. Monday there were no results to be seen. Early Tuesday morning a culture result came back, which was negative. That means that the urine was sterile, as it should be. It also meant that she did not have a UTI. Later that day she got a call from a nurse at the Urgent Care telling her to stop taking the antibiotic because she did not have a UTI.
In summary, my friend’s experience of chlorine dioxide was mixed. Ultimately, it cleared the urinary tract infection, because by week two, before antibiotics, the urine was sterile. For most of the second week, she was without any symptoms, with the added bonus of feeling calmer and not having morning headaches which had plagued her for some time. The reappearance of symptoms at the end of the second week points towards some return of inflammation, but it turned out that it wasn’t because of an infection. It may be that the homeopathic remedy and the numbing medication she had been taking until the end of the second week were doing a good job of keeping those symptoms at bay, and when she discontinued them, there was a mild and brief resurgence. Understandably, without more information, my friend felt discouraged and anxious about the return of symptoms. In retrospect, she wishes she had gone to the lab earlier in the morning and obtained a urinalysis, in which case she would not have started the antibiotic, being reassured that her urinary tract was in fact, clear of infection.
When I spoke to my friend yesterday, I could hear the smile in her voice as she told me that she was thrilled to not have to drink CD anymore. “I can’t wait to get back to my Baobab!”
Ultimately, the labs demonstrated that the CD was effective at clearing the UTI. It wasn’t sufficient to eliminate all of Daisy’s symptoms, but she was able to address that with two other therapies that didn’t harm her microbiome. There were clearly side effects, but they were transient, and there were some unexpected benefits, including an increased sense of emotional calm and improved cognition, which ultimately she described as an improved ability to multitask and not feel overwhelmed. I didn’t expect that. I have proposed to her that we draw her blood and check her microclotting level in in case there is additional information about the impact of CD in breaking down micro clots. She is game for that and I can report the results in the future.
Convenience is king in the United States. I’m inclined to believe that the majority of Americans would not be up for drinking CD every hour for eight hours a day for three weeks. Most people also would not want to contend with the loose stools. Daisy works from home, so this was doable for her. It would be much harder for people in certain occupations where they didn’t have quick and easy access to the bathroom.
One last consideration, which is worth mentioning, is it that Daisy has a history of tick bites. The experts on CD speak to its capacity to effectively treat pathogens ranging from MRSA to tick borne disease. As a vaccine injured person, my friend may very well have reactivated smoldering infections from EBV to Borrelia, not to mention her ongoing spike burden, which, according to her spike antibody testing hovers near 10,000 U/mL, as of her last test results from about five months ago. It could very well be that the diarrhea she experienced in the first week had more to do with the toxins released from killing off reactivated viruses and pathogens than dealing with the UTI itself. We might get some insight into that with further testing.
Many readers will have many questions re: CD. I am a novice student on the topic, as my friend Daisy led the way and was kind enough to share her experience so that I might learn and share it with you. I think it is important to share this case study, because detractors from CD assert that there aren’t clinical trials in humans, treating pathologies. That isn’t actually true, but we can take that up another day. My respected colleague Dr Robert Yoho has poured his heart and soul into writing about all things CD, and I will heartily recommend that you subscribe to his Substack Surviving Healthcare, where you will learn about how CD works, how to purchase it, and how to use it.




Interesting. I have used oregano oil in patients to treat fungal infections (overgrowth in the bowel) identified on stool analysis with Genova Diagnostics. Unfortunately, several patients have developed GI upset within a week of initiating therapy and have needed to discontinue its use.
Good one, Scott, & interesting. Glad she & you shared. Always love reading about baobab!❤️🙏